If you've been in a hospital or visited a patient there you may have seen a nurse administer medication via a needless syringe or by providing the patient with pills. I'm pretty certain it took less than 3 minutes.
What you didn't see are the extra chores they have to do.
The 3 Minute Medication System eliminates several time-consuming chores each nurse has to perform multiple times a day for every patient. This is what we can eliminate:
Imagine eliminating half the time a nurse walks in a shift to find things and medications.
Walking is great exercise, but every time a nurse is walking to find something or someone is time a nurse spends away from their patients. It is no surprise that many nurses on average walk 3 miles a shift - a bit more than an hour spent away from their patients or $60/RN shift. One study reported some nurses working in a unit with a challenging floor plan walked over 5 miles a day.
Besides forcing the nurse to be away from the patient, walking “exposes” the nurse to many distractions. Other nurses stop them to ask a question or to request assistance, for example to witness wasting (see below). Other families request directions to the East Wing elevator and the nurse feels obliged to walk them the hardest to find elevator in the world.
Walking is not a top of licensure activity. Many people with less than a high school education can walk. Of course it is obvious that only a nurse can dispense medications, so walking to get medications is a required part of nursing.
But have we fooled ourselves to accept this waste of time?
Imagine removing the need to audit opiate medication inventory every time a nurse dispenses one, while automatically keeping perfect counts.
Nurses get medications for patients from a unit based automated medication dispenser cabinet (abbreviated as ADC) . These are typically placed in a care unit or shared by nearby care units. They have a variety of locked drawers and sub-compartments, each storing multiple doses of the same medication. A nurse electronically selects a medication and the correct drawer is unlocked, opened, and the correct sub-compartment is identified. When a nurse is dispensing an opioid medication (often a syringe or sealed vial) they first have to count the contents of the sub-compartment with . This is a blind count, since they do not know the previous count by the prior nurse who obtained an opioid from that sub-compartment
When done the nurse enters the number into the ADC. If there is a discrepancy from the previous nurse's count minus the dose(s) they took, a nurse manager or pharmacist will have to sort out the cause for the difference. The prior nurse and the current nurse will be interviewed to determine why there is an audit error. This consumes time for all involved and may include a video playback of each of them using the ADC. It is quite uncomfortable for both nurses who are considered as possible opioid thieves. A “judicial” conclusion is challenging as audit mismatches don’t directly provide legal evidence just that someone may have entered an incorrect number or taken an extra dose.
 Typical Automated Dispensing Cabinet
Typical Automated Dispensing Cabinet
When this discrepancy is detected at the beginning of a shift the prior nurse has already left for the weekend and won't be interviewed until the next week. By then their memory of dispensing a medication may be less than perfect.
Counting 3 or 4 items is easy, but when there are 20 or more it takes time and a miscount is always possible.
Nurses dislike having to be the medication auditor multiple times a day.
Walking from the patient to get medications is one of the most common reasons nurses leave their patients room, adding to time a nurse walks every shift. Not only do nurses have to walk to the cabinet, often during the first hour of the day shift they will find a line of other nurses waiting for the "early bird" nurse to finish dispensing medications for their patients and to conduct blind counts as needed. The alternate is for the nurse to walk back to their patients and later walk back to the cabinet to dispense the medications their patient needs. When a sub-compartment that holds medication they need is empty the nurse will have to walk to the nearest alternate medication cabinet to see if it has that medication - adding additional walking and time.
Walking and waiting for the care unit's medication cabinet is so time consuming that nurses have been allowed short cuts such as being able to dispense medications for 2 patients at the same time or dispensing morning and noon medications for the same patient. Neither of these are safe situations and can encourage adulteration or theft of dispensed controlled substances. A nurse carrying multiple controlled substances for a long time provides them the opportunity to use a restroom and self-dose from a for a patient syringe and replace the missing volume with water. This has been a common way for patients to acquire Hepatitis-C in a modern hospital.
It is always dangerous to share syringes.
Imagine not having to wait and wait to find a free nurse to witness wasting opioid medications while being able to verify the waste has not been substituted with water.
In 2014 the DEA (Drug Enforcement Agency) ruled that healthcare facilities had to render residual or unused controlled substances into a “non-retrievable” form, which some thought flushing them into a toilet would work. In 2019 the EPA (Environmental Protections Agency) also ruled that unused or residual medications could no longer be flushed down a toilet as the water system was being polluted with medications from hospitals and other care centers.
This resulted in products like the Cactus Sink and Rx Destroyer that used canisters of liquid chemicals to treat unused or residual medications including controlled substances. These canisters are placed in the unit medication room or at nurses’ stations and are typically locked to a wall or counter surface.
A nurse who administered who has residual controlled substance in a syringe after patient administration would walk to find another nurse (more walking) to act as a witness. If all nurses are occupied the nurse returns to their patients and waits for a second nurse to be free. When the nurse finds a free nurse (not easy to do in busy units) they both go the canister where the nurse would eject the residual controlled substance medication into the canister as observed by the witness nurse. Both nurses have to document that a residual 1ml of morphine was “wasted” from a syringe at that date and time in the electronic record. All this takes precious time and keeps 2 nurses away from their patients.
 2 nurses while wasting controlled substance
2 nurses while wasting controlled substance
Besides being time consuming the witness nurse has no idea if the syringe or IV bag has opioids or just water.
It is no surprise many waste witnessing occurs at the end of the end of shifts, especially in busy units. This leaves the nurse in possession of the controlled substance for hours. This has been used by addicted nurses as time for them to slip into a restroom self-inject the residual controlled substance and refill the syringe with water.
When a nurse is available for witnessing, that nurse can really only determine that the first nurse is wasting (ejecting) a clear liquid substance into the canister. The witness nurse presumes it contains morphine, but has no way to know if it is only water. The witnessing process has nothing to do with security as it is a theatrical performance.
When nurse is an honest nurse then witnessing is not needed and when a nurse is addicted it is not effective other than to waste time.
To top it off the chemicals used in one of the most common brands do not destroy controlled substances as they only include vomit-inducing substances and embitterments to cause a person attempting to swallow the liquid it to immediately spit it out or vomit. Those canisters are rendered non-retrievable by sending them to licensed biowaste incinerators.
Imagine the time saved when all the electronic records related to nurse medication dispensing, administration, and waste are automated.
Documenting every nursing activity is essential to keep the entire medical team caring for the patient aware of the patient’s current status.
However, to administer medications a nurse will have to document the medications dispensed from the medication cabinet including the blind counts when required. When at the patient, the nurse has to electronically document each medication and the amount given to the patient. When using a syringe the actual amount can vary as the medication concentration and the volume dispensed can be larger than the ordered amount.
For controlled substances there is a third step that requires documentation, see Witnessing the destruction of controlled substances (described above).
Nurses are not the only ones with a documentation burden. Pharmacy technicians who load medication cabinets in a hospital have to count and document the number of doses or items in a sub-compartment when it is opened to be refilled and count the number of new doses they insert in it. While this can take time it does not involve a reduction of the time nurses spend with patients except when a nurse arrives at the medication dispensing cabinet and it is being refilled. In that case the nurse may have to wait for pharmacy technician to complete the counting and refilling of a medication compartment. The technician should be given the same courtesy as the nurse to complete their medication work without distraction.
 Davey Do/All Nurses
Davey Do/All Nurses
Imagine the time saved when nurses no longer have to wait in line for other nurses to finish dispensing medications or to wait for another nurse to act as a witness.
This is possible when each nurse has immediate access to a medication dispenser
Going to the automated medication cabinet to dispense medications for a patient and finding several nurses already in line is frustrating. You either wait for the others to dispense medication for their patients (and to blind count audit compartments as needed) or you return to your patients go back to the dispenser in 15 minutes. No one likes to wait in lines, but nurses can frequently experience lines.
Nurses don't wait in a line to waste residual or unused opioid medications, but they have to wait to find a free nurse to observe wasting these medications into a communal canister. In a busy or understaffed unit it is no surprise that many wasting events get pushed back to the last hour of the shift as all wasting has to be complete before the shift is over. Think of a process that allows nurses to waste and destroy opioid medications at any time in the patient's room.
The 3 Minute Medication™ system starts with the Interactive Waste Collector™ (IWC). This addresses multiple weakness and problems of residual opioid wasting that is common to all hospitals.
The IWC introduces a process to waste residual Controlled Substances that is traceable back to a specific syringe, nurse, and time. Wasting residual a controlled substance is done immediately after medication administration. However, it allows any residual medication in a syringe to be assayed by Pharmacy Services using analytic instrumentation provided by Oparus. The pharmacy staff acts as the witness, freeing the administering nurse from having to spend time finding a witness nurse observer and documenting their action in hospital databases. Instead pharmacy services is able to verify the medication, quantity, and concentration that was wasted while promptly detecting any adulteration/diversion of Controlled Substances.
This creates a traceable chain of custody for any medication syringe that needs to be preserved as evidence. The process also ensures Controlled Substances that have been verified are rapidly destroyed within the hospital to the DEA “non-retrievable” requirement and does not require incineration as required for common opioid wasting products. When done the syringe and destroyed contents are recycled.
 10 ml and 2ml waste cartridges with syringes and NFC label
10 ml and 2ml waste cartridges with syringes and NFC label
It starts with our controlled substance waste cartridges. These are miniature chemical laboratories. Cartridges are available in 2ml, 10ml, and 50ml sizes suitable for common syringes and one mini IV bag. These are used immediately after administration in the patient room when there is residual controlled substance in a syringe. The nurse attaches the syringe to the Luer lock connector of the cartridge and ejects the residual medication into the cartridge.
To track the cartridges each has an embedded NFC (Near Field Communications) label. This is a smaller version of RRID labels and provides each cartridge with a random and unique serial number for identification and tracking purposes. NFC labels are more expensive than bar codes, but can't be duplicated by cell phone camera like bar codes. Bar codes are identical for every syringe with same medication, form, and concentration
For best security the controlled substance syringes should also have an NFC label attached in pharmacy or by the manufacturer. It identifies the syringe medication, concentration, volume, expiration, and date filled (when filled by pharmacy from a sealed vial).
Chemicals in the cartridge start to destroy the controlled substance to the non-retrievable DEA rule in minutes. However, trust but verify is always important (but not possible with canisters). Some of the cartridges have only water and no chemicals. The controlled substance in these cartridges are not destroyed and are reserved for chemical analysis at pharmacy services. As each cartridge is linked to a specific syringe and a specific medication, concentration, and volume the assaying at pharmacy services is automatically adjusted to detect that chemical signature for that medication.
The number of cartridges without chemicals can vary from 5% to 100%, depending on whether pharmacy wants to test some or all cartridges from a unit.
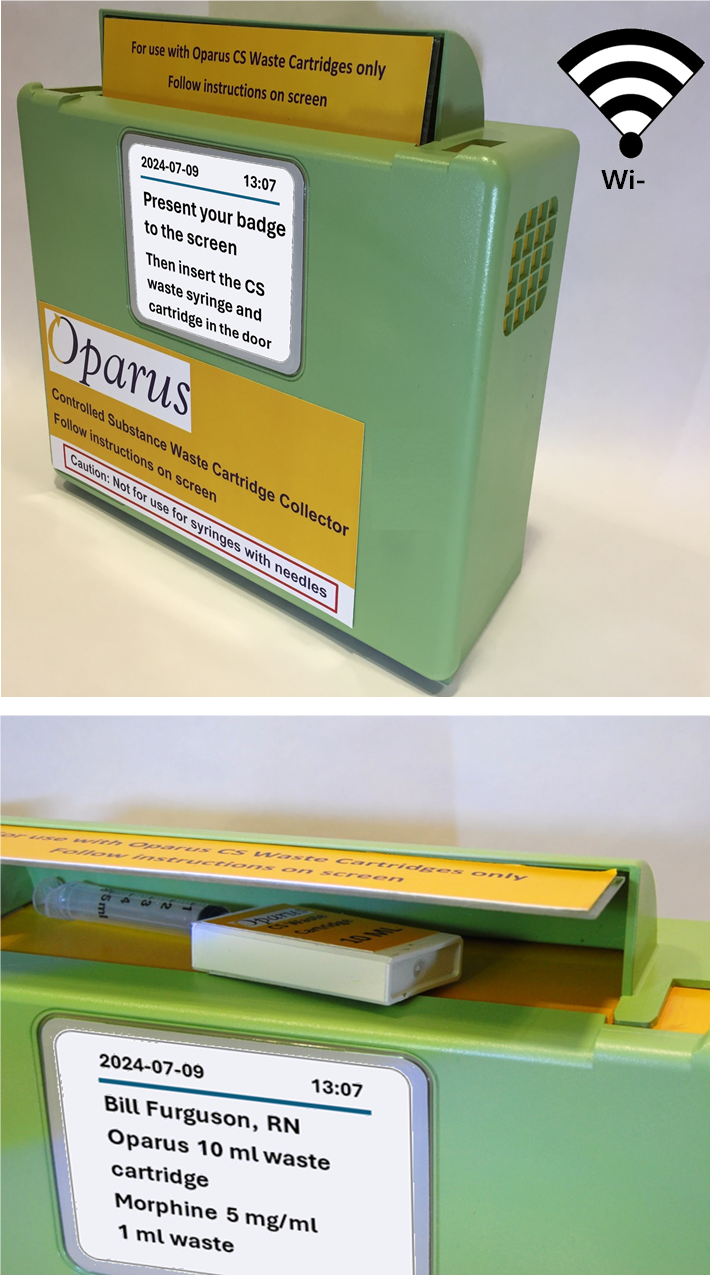 Interactive Waste Station with cartridge and syringe inserted
Interactive Waste Station with cartridge and syringe inserted
Next the nurse takes the cartridge and the emptied syringe to the medication room or the nurses’ station. The nurse presents their badge, which also has an NFC label embedded in it, to the IWC. The IWC unlocks the top door, the nurse inserts the waste container and the emptied syringe into the interior of the IWC validation chamber and closes the door.
The IWC the reads the NFC tags of the syringe and the cartridge. If the serial numbers are not recognized, for example someone trying to use a non-hospital NFC tag or no tag is present the IWC will reject the items. The IWC reopens the top door and requests the nurse to remove the items. The IWC will also reject syringes with needles attached unless the syringe has been locked in a recognized protective, non-removeable cover.
When accepted the cartridge and the emptied syringe are weighed in the validation chamber. All aspects of this process are sent to a computer in pharmacy services.
Finally a trap door at the bottom of the validation compartment is unlocked and opened allowing the cartridge and the syringe to be dropped into the IWC body.
It is recommended that the nurse also uses the IWC when there is no residual waste and no cartridge is needed. Using the IWC ensures that every controlled substance syringe (with or without a residual volume of medication) is tracked as it leaves pharmacy, is used, placed in the IWC in timely manner shortly after administration, and returned to pharmacy. This automates the DEA requirement that every dose of controlled substance be accounted for.
The benefit is all syringes are accounted for by being placed in the IWC at the end of the shift. In reality controlled substances should be dispensed when the nurse is ready to administer them, so a long time between dispensing and disposing in the IWC can indicate theft or adulteration. Controlled substance syringes and IV bags can't be taken home to be refilled or for self-injection without detection. The recent adulteration of 50ml IV bags at the Rogue Valley Medical Center involving multiple patient deaths would not be possible as we track IV bags as well.
The IWC is electronically operated by a nurse using the interactive touch screen. Also supported is Wi-Fi communications to pharmacy service and automatic detection of any attempt to force open or to remove the IWC from its wall bracket. When removed by an authorized pharmacy technician the IWC remains in communication with pharmacy services using a built-in battery and can be route tracked while in a transport cart.
The IWC automatically creates a report identifying the nurse, the medication, the amount waster, the specific waste cartridge status used, and the date and time the cartridge and syringe are accepted by the IWC. The nurse only has to confirm the report or add any special observations.
Every hospital room has a sharps container, so it is natural to think there should be an Interactive Waste Collector™ (IWC) in those rooms as well. We thought the same but with the level of electronics and security they have we quickly thought what else could it do to support nurses and eliminate time wasting shores they face.
 Patient Centered Medication Station
Patient Centered Medication Station
So we developed the Patient Centered Medication Station™ or PCMS. The PCMS fully enables the 3 Minute Medication™ system to save nurses the most time. It has all of the features of the IWC scaled down a bit in size, but there is a lot more. We added a medication dispenser to the left of the waste collector. It is designed to hold a 2-day supply of all the medications a typical patient needs in each unit or used for a procedure room. The PCMS does not replace the sharps container as the waste collector section, as described above, as it does not accept syringes with needles unless they are locked in a recognized protective, non-removeable cover.
The touch sensitive 10" display is there, but larger to provide nurses additional information to nurse about the medications. Again Wi-Fi and Bluetooth communications are included. Just like the IWC, the PCMS uses NFC labels to keep track of the medications loaded by Pharmacy Services and when they are removed by a nurse in the patient's room.
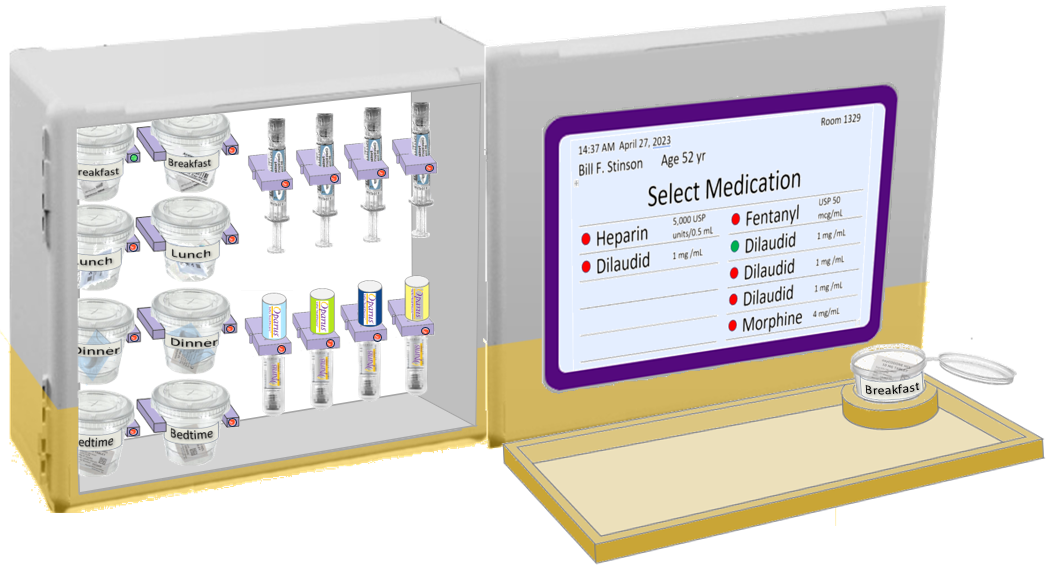 PCMS dispenser door slid open - 2 day medication supply
PCMS dispenser door slid open - 2 day medication supply
There is an electronically locked door with detectors to sense if the is an attempt to force the door open. The PCMS is easily electronically unlocked and removed from its wall mounting bracket by a pharmacy technician and replaced by newly filled PCMS. The PCMS and the IWC as transported by smart carts that allow the PCMS to be slid in a locked during transit. The cart knows the room filled PCMS is go and assists the transport pharmacy technician to follow the most efficient route to those rooms.

The PCMS is modular so it can be configured to meet the needs of an ICU, step down unit, and procedure or operating room. Being modular it can hold 2ml to 60ml syringes, sealed vials, IV bags, solid oral medications, vials, patches, and waste cartridges as described above.
Automated Dispensing Cabinets are accessed by every nurse in the unit and by pharmacy technicians that refill them. During a busy shift the dispenser can be opened 30 or more times. There are multiple weaknesses in these machines that have been exploited. For example it was possible to remove controlled substances and replace them with fraudulent look-alike medications or replaced with syringes or IV bags drained and refilled with water. Too often no one was the wiser.
The PCMS is different as each is assigned to specific patient and it is also assigned to the nurse assigned to that patient during each shift. During their shift only that nurse has full access to the PCMS. Of course the unit nurse manager will also have access if needed and can reassign access if the nurse is called away or has been assigned to a different unit. A second nurse on each shift can also have access to the PCMS when the primary nurse is off the floor, for example during a meal. However most nurses would prefer to administer any medications ordered for their patients before they leave the floor. So each PCMS is really accessed by one nurse per shift.
No pharmacy technician has access to the PCMS outside the pharmacy where the PCMS loaded. The pharmacy technician delivering filled PCMS or removing emptied PCMS has no access to the interior of the dispenser when away from the pharmacy.
Every time the assigned nurse or rarely the secondary nurse uses the PCMS their identity is verified and recorded along with the medications removed. Similarly the waste cartridges and used syringes inserted into the waste collection section of the PCMS. Every transaction is transferred to a pharmacy audit and analysis server from Oparus and automatically shared with the hospital electronic health record system.
The PCMS does everything that is needed to save nurses from meaninglessly wasting time. It eliminates: