Oparus makes hospital medication administration safer for patients, nurses and other healthcare workers. Medication administration is the most common therapeutic activity for nurses, but it comes with multiple challenges and anxieties related to locating each medication, dosing, timing, and in some cases transferring from a sealed vial into a syringe before administration.
Even with decades of experience in patient safety our team learned something new. In order to make healthcare safer – healthcare naturally became faster. We are not interested in seeing if nurses can work faster or put them on a virtual endless treadmill going faster. Instead we found that eliminating useless activities (more like chores) and adding new technologies that are often invisible we could return precious time to nurses to be at their patients’ bedside, providing what they became nurses to do - care for patients.
We aren't the only ones to think this way. Dr. Richard Shannon a cardiologist and member of the Board of Directors at Kaiser Foundation Health Plan has commented on why nurses don't have time to be nurses:
“We found nurses doing valuable work only about a third of the time.
The rest of the time they are doing work that has little value or
is a complete waste of time.”
Dr. Shannon is telling us that on average during a 12-hour shift hospital procedures waste 8 hours of nurses’ time every day. Work that should be done by someone else or not at all. Time wasted administering medications alone is 20% of a 12-hour shift and often much more. Doing the arithmetic this is $144 of wasted time per shift and is what we concentrate on.
For 2022 the Bureau of Labor Statistics (BLS) posted the national average salary for a registered nurse was $42.80 without benefits. A new table includes salary and all benefits, overtime, training time, and employer taxes states the average to be $71.09/hour, more in California and less in Louisiana. BLS web site see Table 4 for Register Nurses
For simplicity we use a cost $1/minute ($60.00/hour) for nursing time.
It is easy to argue that we do not have enough nurses to provide the safest medication care. However many believe we have enough nurses, but have shackled them with too many non-nursing activities that are worthless to patient care. This includes activities we think a nurse should do, but we just haven't considered alternatives to eliminate the need for a nurse to do that work.
Over the past 20 years more and more non-nursing “chores” have been added to nurses’ jobs especially when administering medications. These chores keep the nurse away from the patient room. Many of these chores were established with good intentions to improve care, but too many were activities that nurses recognized were not just ineffective, but allowed patient care to be unsafe when shortcuts and overrides are involved in an attempt to save time.
Medications for pain control (generally controlled substances or opioids) are probably the most commonly ordered medication in a hospital. They also come with the greatest burden of extra chores. A rule of thumb is each patient on average will be given 2 doses of an opioid a day. Yes there are some patients that aren’t prescribed any opioids, but others will receive 3, 4, or more doses a day. When handling opioids nurses are plagued by even more additional time-consuming chores.
Adding nursing chores is linked to two major issues in healthcare - poor patient safety and nursing dissatisfaction with their jobs.
When nurses are away from a patient, the patient tends to be discharged later patient and will more likely experience safety issues. Nurses occupied by other patients delay giving medications, sometimes by hours, a medication error that no nurse wants to cause. Even when nurses are in a patient's room they are subject to endless distractions and interruptions (text message, voice pagers, and technicians and other staff with questions). Nurses are challenged to maintain situational awareness, increasing the opportunity to skip a step or forget a procedure, resulting in poor or dangerous patient care.
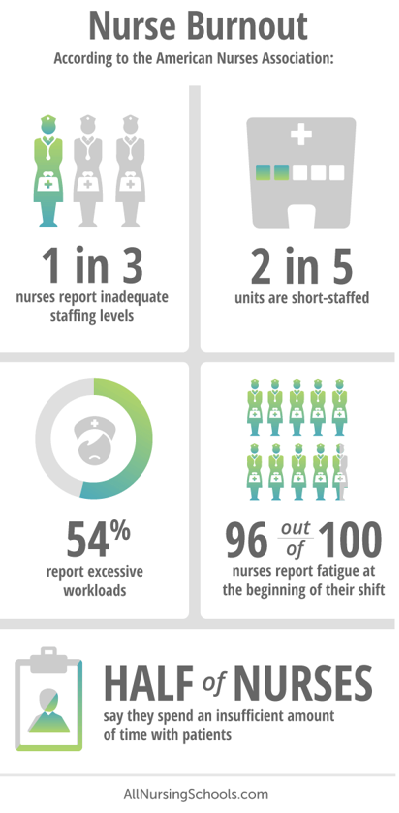
Nursing dissatisfaction with their profession has grown markedly in the past few years. Some are related to the negative aspects of being a front-line health professional during Covid-19. But this is not all of it. A well-known issue is when nurses are consumed by chores (that someone with a high school education could do) they are clearly not working at the top of licensure. Being held responsible for patient care when they are frequently absent is frustrating.
Everyone has heard of burn out, often no longer willing to work in a defective system. Recently a new phrase has arrived - "rust out". This is used to describe working for a long time in a position that doesn't challenge your professional skills. Rust was chosen as the descriptor, as in your skills become rusty or corroded from lack of use. There are countless nurses experiencing rust out.
Nurses salaries have increased significantly in the past year. One hospital awarded $100,000 retention bonuses to nurses who agreed to stay for 3 years. If you have a system that people don't want to work in, this may temporarily work at the risk of crushing the hospital’s financial margins. One survey states 31 percent of nurses say they intend to leave direct patient care jobs in the next year, so perhaps a bonus the size of a house downpayment may be needed to keep them.
Every nurse knows they can book a flight to Hawaii with a hotel reservation in 15 minutes, but at the hospital what can they get done in 15 minutes? Well a lot if they aren't held back.
To find out exactly what is holding them back go to our 3 Minute Medication™ system tab.
Over New Years weekend 2024, it was reported that a nurse in 2022 working at the Rogue River Medical Center in Medford, Oregon had removed the contents of 50 ml IV bag containers of fentanyl and refilled the missing liquid with tap water (obviously not sterile). This became a mass murder when a reported 9 or more patients died - publicly released information is limited. As these were ICU patients many with complex medical histories and deaths in the ICU or afterwards are not uncommon. The hospital probably did not understand what was occurring in 2022 and was unequipped to prevent additional injuries.
As you would expect the hospital management was “distressed to learn of this issue”.
An unknown number (dozens) of patients were also administered the adulterated IV bags and survived They may have been healthier or were infused with a lower volume, but clearly did not receive their ordered pain relief.
It is alleged that the tap water contained pseudomonas which can cause sepsis, pneumonia, and organ failure. Many have questioned why the hospital tap water contained this bacteria, but neglect to consider the nurse who did this may have taken the IV bags home and filled them with water from a private well and returned them to the hospital.
In polite society this is referred to as “diversion”. You probably associate the word diversion with a new traffic detour due to construction. In ordinay English we use uncomplicated words to refer to diversion in clear understandable words like - “theft” or "stealing" or "adulteration".
Here are a sample of appropriate headlines:
No one can figure how this could have happened or how in December 2023 the hospital could determine patients that died 18 months earlier had been died due to aninfectin from adulterated IV bags.
UPDATE June 13, 2024 A nurse was arrested and charged with 44 counts of assault in the second degree. Of these patients 16 died, but charges of murder were not filed. This is probably beacuse conclusive gounds to chrage murder or manslaughter is difficult to establish when patients died months earlier. Likely there is no contemporaneous evidence collected and retained and no one witness the diversion exist. After all hospitals are not in business of collecting evidence of murder. This leaves relatives of patients who died to pursue the nurse and the hospital in civil court for wrongful death. At least one such suit has been filed.
Jackson County Chief Deputy District Attorney Patrick Green reported “Investigators in this case consulted with numerous medical experts who were all unanimous that they could not conclude that any of the patient’s deaths were directly attributed to the IV bags.
A national problem
The NIH, The Joint Commission, and others estimate 10% to 15% of healthcare workers will misuse drugs during their career. Some of them care for patients every day in your hospital and when the opportunity arises, they will destroy every bit of the safety goals you have by diverting (stealing) Controlled Substance medications.
Commander John Burke at the Cincinnati Police Department lead the most focused team in the country to find the workers, arrest them, get them into recovery, and place them back into healthcare roles. He was told that he would never find an opioid thief in a children’s hospital as all professional workers were mission driven, wet that is exactly where he found most of his initial staff to arrest.
He extrapolated from his work that there should be 37,500 healthcare workers arrested a year for stealing opioids, but only a few hundred are. This is not the total number of drug abusers in hospitals. It does not include healthcare workers that are so well practiced that they have never been found.
The reality is all hospitals are unable to prevent or detect this theft.
Hospitals want to make medication administration safer.
If you think this is an aberration then consider the Yale Medical Fertility Clinic in 2021. Exactly the same situation, a nurse replacing 50 ml fentanyl IV bags. Now there were no infections because the bags were refilled with sterile water, but an unknown number of women were subjected to extreme pain, for what is normally a painless procedures. Reports state that 74 women are suing Yale Medical for $114 Million.
Then there is the case of an anesthesiologist at Baylor Scott & White Medical Center who injected various medications into an unknown number of sterile IV bags in 2022. The adulterated bags were replaced into the stock supply for use in surgical procedures - effectively as toxic medication time bombs to be used on random patients.
The adulteration was first suspected when a normal 18 year old patient was sent to the ICU following routine sinus surgery. His presentation at the ICU included high blood pressure, cardiac dysfunction, and other symptoms. Suspicion about this event and other anomalous cases resulted in a request for the lab to analyze of the remaining contents of the IV bag. This revealed revealed a combination of a nerve-blocking agent, a stimulant, and an anesthetic. In retrospect other patients suffered cardiac emergencies during routine procedures. Subsequently a doctor died of cardiac arrest when she used an adulterated IV bag to self-treat her own dehydration.
The anesthesiologist was convicted on 10 counts and faces a life sentence.was convicted on 10 counts and faces a life sentence.

Or consider the gastroenterologist who by reusing propofol bottles causes the spread of Hepatis C and HIV resulting in the death of 2 patients and 40,000 others were recommended for blood testing. Why were so many patients to be tested? Because the sharing of vials and syringes had been undetected for so long there was no way to determine who might have been affected, so every patient over several years could have been infected.
As you might expect many lawsuits came from this. A group of patients were awarded $500,000,000 by a jury.
Medical centers do not now have the tools to prevent or detect all theft of opioids and syringe reuse.
There has been a major emphasis on improving patient safety in hospitals since the 2000 report by the Institute of Medicine "To Err is Human: Building a Safer Healthcare System" which asserts that medication errors are not due bad people in healthcare - it is good people are working in bad systems that need to be made safer.
The IV bag adulteration discussed above informs us that there really are "bad" people working in "bad systems" who will destroy safety goals. In this case the "bad systems" don't just make it challenging for good nurses to be nurses, they also allow controlled substance theft and adulteration to be undiscovered until patients are injured or die.
We need to do better than merely hope patients will be safe in our care.